Ezer Dry Eye Sapphire A+
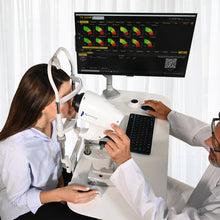
The Sapphire A+ Device is the new instrument for the individual analysis of tear film that allows to carry out a quick detailed structural research of the tear composition. Research on all the layers (Lipid, Aqueous, Mucin) and Meibomian Glands. Thanks to the Sapphire A+ Device it is possible to identify the type of Dry Eye Disease (DED) and determine which components can be treated with a specific treatment, in relation to the type of deficiency.
*Purchase includes one software license
$4,968,649.24 $2,104,879.60
The Sapphire A+ is designed to perform tear film tests, from the quality of tears to the analysis of the Meibomian Glands. Is the new instrument for the individual analysis of the tear film that allows to carry out a quick detailed structural research of the tear composition.
All in One


Evaluation of all Tear Film Layers


Fully Automatic Protocol


EXAM DESCRIPTION: AUTO INTERFEROMETRY
The Sapphire A+ automatically evaluates the quantity and quality of the lipid component on the tear film. The device highlights the lipid layer and the software analyses automatically Lipid Layer Thickness (LLT).

AUTOMATED LIPID LAYER ANALYSIS
The evaluation of the lipid layer is part of your overall Dry Eye Assessment. Knowing what is causing Dry Eye will help determine the best treatment option. After your assessment is complete, the Optometrist will discuss your treatment options. Lipid pattern classification, incidence and clinical interpretation is adapted from Guillon & Guillon description incidence (%) with estimated thickness (nm).

Observation of blinking frequency and completeness should also be considered - while listening to history and symptoms can be an ideal time to observe this. A typical blink pattern can be observed as approximately one blink every five seconds, ie 11 blinks per minute. Incomplete blink can often be observed in contact lens wearers, and frequent blink may be a result of an attempt to maintain a relatively thin lipid layer.

The software automatically detects the coloured lipids on the patient’s eye and determines lipid layer thickness (LLT).
In a few seconds it is possible to get automatically relevant data to understand functionality of Meibomian Glands such as average LLT.
EXAM DESCRIPTION: TEAR MENISCUS
Low tear production may result in aqueous tear deficiency (ATD) and cause dry eye symptoms. However, measuring the tear volume is difficult since the methods normally used are invasive and irritating.
Reflex tear production can be induced, giving an overestimation of basal tear flow and volume. The sizes of the tear meniscus are related to the tear secretion rate and tear stability, and they are good indicators of the overall tear volume. Tear meniscus height is related to the tear secretion rate and tear stability and for this reason it’s a good indicator of tear production.
The aqueous layer is evaluated through the noninvasive “Tear Meniscus” test and is then classified into different categories.
The Sapphire A+ Device is an excellent method of screening for dry-eye patients, to measure the upper and lower tear meniscus in patients with aqueous tear deficiency (ATD) dry eye and to determine the most effective meniscus variables for the diagnosis of dry eye. Normal tear volume is important for the maintenance of ocular surface physiology and ocular comfort.
The total tear volume is composed of the tear meniscus, which contains 75% to 90% of the tears, the pre-ocular film and the cul-de-sac. Recent advances and associated software have enabled the simultaneous imaging of both upper and lower meniscus, and real-time changes have been reported.

AUTOMATED LIPID LAYER ANALYSIS
With the various magnification tools, it is possible to measure the tear meniscus height on the lower eyelid and evaluate its characteristics.
With the various magnification tools, it is possible to measure the tear meniscus height on the lower eyelid and evaluate its characteristics.
The result of this exam is comparable to the Schirmer’s Tear Test 1 (STT1), with the difference that it is not invasive and lasts 3 seconds instead of several minutes.
EXAM DESCRIPTION: AUTO NIBUT
The stability of the mucin layer and the whole tear film is assessed through the study of non-invasive break up time (NIBUT), by using the Placido cone projected onto the cornea.

The Sapphire A+ Device allows to evaluate tear film stability and regularity, using non-invasive break up time measurement (NIBUT). This measures the number of seconds between one complete blinking and the appearance of the first discontinuity in the tear film.
With the Sapphire A+ Device, thanks to one single video, the physician can gain lots of information:
• Automatic NIBUT
• Average of more than one value
• Graph to understand the trend of tear film stability during the video
• Tear topography that shows all breaking the tear film during time.

TEAR STABILITY EVALUATION
Through Placid disk projection on patients’ cornea, TFA automatically evaluates tear film stability. The software checks periodically cornea’s shape with the Placid rings and detects any deviation, providing break up time values in an easy and understandable way. AVG BUT is provided with normograms and, after different analysis, shows the trend line for a useful follow up after treat.
Through the Placido rings, TFA automatically provides:
• First BUT
• Avg BUT
• Stability graph
• Tear topography
EXAM DESCRIPTION: EYE BLINK
It has been established that efficient blinking plays an important role in ocular surface health including during contact lens wear and that it improves contact lens performance and comfort.

A healthy person should be expected to show periodic blinking, by closing the eyelids briefly.
Most blinks are spontaneous, occurring regularly with no external stimulus. However, a reflex blink can occur in response to external stimuli such as a bright light, a sudden loud noise, or an object approaching towards the eyes.
A voluntary or forced blink is another type of blinking in which the person deliberately closes the eyes and the lower eyelid raises to meet the upper eyelid.

A complete blink, in which the upper eyelid touches the lower eyelid, contributes to the health of the ocular surface by providing a fresh layer of tears as well as maintaining optical integrity thanks to a smooth tear film over the cornea.

The rate of blinking and its completeness vary depending on the task undertaken during blink assessment, the direction of gaze, the emotional state of the subjects and the method under which the blink is measured.
It is also well known that wearing contact lenses (both rigid and soft lenses) can induce significant changes in blinking rate and completeness.
It is been established that efficient blinking plays an important role in ocular surface health during contact lens wear and that it improves contact lens performance and comfort.
Inefficient blinking during contact lens wear may be related to a low blinking rate or incomplete blinking and can often be a reason for dry eye symptoms or ocular surface staining.
TFA automatically detects and analyses blinking, determining its quality.
EXAM DESCRIPTION: MEIBOGRAPHY
Meibography is the visualization of the glands through illumination of the eyelid with infrared light. It images the morphology of the glands in order to diagnose any meibomian gland drop out which would lead to tear dysfunction.
MEIBOMIAN GLAND AUTO DETECTION ON UPPER AND LOWER EYELIDS
Meibomian Glands (MGs) play a significant role in tear quality by producing lipids (meibum) that are part of the superficial tear film. Dysfunction of the MGs destabilizes tear composition resulting in evaporative dry eye.
Meibomian Glands (MGs) play a significant role in tear quality by producing lipids (meibum) that are part of the superficial tear film. Dysfunction of the MGs destabilizes tear composition resulting in evaporative dry eye.
The posterior lamella of the eyelid hosts a fleet of parallel MGs situated between the palpebral conjunctiva and tarsal plate. A normal Meibomian Gland is approximately linear and 3–4 mm in length, traversing the posterior eyelid perpendicularly to the lid margin. Closer inspection of a Meibomian Gland demonstrates a tubulo-acinar architecture with saccular arrangements of acini and a ductal system that communicates with orifices near the muco-cutaneous junction of the eyelid.
Glandular acini contain clusters of modified sebaceous cells called meibocytes (functional unit of the Meibomian Gland).
These cells synthesize and secrete lipids (meibum) into the pre-corneal tear film. Meibum permeates the tear surface where it serves several important functions. It prevents tear evaporation and thus desiccation of the ocular surface; it acts as a physical and hydrophobic barrier to the inward movement of environmental and organic agents; and it lubricates the ocular surface to prevent irritation while promoting a clear ocular image. Consequently, tear physiology is dependent upon the proper functioning of the MGs.
THE SAPPHIRE A+ DEVICE CAN DETECT THE LENGTH AND WIDTH OF MEIBOMIAN GLANDS SHOWN THROUGH INFRARED MEIBOGRAPHY WITHOUT REQUIRING ANY INPUT FROM THE USER. THE IMAGES ARE THEN AUTOMATICALLY CLASSIFIED.

HOW IT WORKS
The System automatically analyses the images taken through a sensitive infrared camera (NIR) to locate the Meibomian Glands in a guided way:
The System automatically analyses the images taken through a sensitive infrared camera (NIR) to locate the Meibomian Glands in a guided way:
• An exam valid both for the upper and the lower eyelids;
• Automatic percentage of the extension of MGs in the chosen area
• Automatic percentage of the Meibomian Gland loss area If the operator prefers, it is also possible to manually compare the images taken with three different related grading scales.

AUTOMATIC LID DETECTION
To decrease evaluation time, the software automatically detects the lid margin for MG analysis.
To decrease evaluation time, the software automatically detects the lid margin for MG analysis.
Meibomian Gland dysfunction (MGD) is characterised by chronic, diffuse abnormalities of the Meibomian Glands and altered secretion and chemical composition of meibum. MGD leads to increased tear evaporation, increased tear osmolarity and an increased susceptibility to ocular surface inflammation, epithelial damage and discomfort. MGD is the leading cause of dry eye disease and affects most of the population.
Blepharitis is a common eyelid condition that can lead to symptoms ranging from burning, to itching, flaking, eyelid discharge, eyelid redness, and the occurrence of frequent "pink eye"-like flare ups.

Different evaluations should be performed on Meibomian Glands in order to prescribe the most appropriate treatment, such as Intense Pulsed Light (IPL). The Sapphire A+ tools allow an accurate comprehension of the ocular surface and especially the Meibomian Glands. The acquired images are processed and transformed into 3D pictures.
Thanks to scientific algorithms it is possible for the physician to see these 3D images, and to show them and explain abnormalities to the patients.
It will therefore be easier for the physician to recommend a specific treatment even if it is more expensive. It will also be possible to evaluate the efficacy of periocular intense pulsed light therapy on MGs.
EXAM DESCRIPTION: MEIBOGRAPHY 3D
This new imaging system provides strong evidence to support the choice of a specific therapy (for example IPL treatment) and helps the patient to understand why a certain therapy is being recommended.

AN OUTSTANDING DIAGNOSTIC EVALUATION IS NEEDED TODEMONSTRATE THE EFFECTIVENESS OF THE IPL TREATMENT TO PATIENTS
The revolutionary introduction of the 3D Meibomian Gland imaging gives two big advantages. Firstly, it enables to confirm the presence of abnormal glands compared to a healthy subject in a 3D view; secondly, it provides a clear image to share with the patients, to help explain the potential reason of their discomfort.
Moreover, this new imaging system provides strong evidence to support the choice of a specific therapy (for example IPL treatment) and helps the patient to understand why a certain therapy is being recommended.

BENEFITS FOR PATIENTS
• For the first time, a 3D image can help to understand the structure of the eyelids. It can show possible diseases of Meibomian Glands and differences with healthy MGs.
• Patients can see for themselves why they are getting eye discomfort and fluctuating vision.
• Patients can understand why a specific treatment is suggested.

ADVANTAGES FOR THE PHYSICIAN
• Viewing the presence of abnormal gland structures in a high-resolution 3D image.
• Comparing a normal patient gland profile with that of an MGD patient.
• Evidence that supports the diagnosis in the case of evaporative dry eye disease and the explanation of the reasons for the choice of MGD therapy (including IPL).
• Compelling evidence to help the patient visualise what is happening to the Meibomian Glands.
• Providing the reassurance that MGD is a contributory factor in the diagnosis of evaporative dry eye disease.
EXAM DESCRIPTION: BLEPHARITIS AND CYLINDRICAL DANDRUFF
This test helps to visually see blepharitis and presence of Demodex. It can be performed on the outer surface of the eye and eyelids.

The human skin surface is known to house millions of bacteria, though some people have more than the normal and healty quantity. Blepharitis is an inflammation caused by some bacteria that lie at the base of eyelashes. They produce dandruff-like flakes in the skin, which lead to infection and inflammation.

Problems with the Meibomian Glands (meibomianitis) in the eyelids can also cause blepharitis. The development of inflammation is also associated with risk factors such as dandruff, dry eye, acne rosacea, or bacteria. Blepharitis is a common eye disorder affecting all age groups. The eye must be evaluated using a specialized tool such as the Sapphire A+ magnifying device. This tool highlights inflammation in the eye and the existence of bacteria/fungi/viruses.
If signs of infection are found during close monitoring, the ophthalmologist wipes the eye and collects any discharge as a sample. This is then evaluated under a microscope. Comprehensive Eye Examinations.

This test helps in the detection of blepharitis. It can be performed on the outer surface of the eyeball and eyelids.
The process includes:
• Analysis of the patient’s history.
• Extrinsic detection of the eye structure, skin texture, and appearance of eyelashes.
• Examining the openings of the Meibomian Glands, base of the eyelashes, and eyelid margins using a bright light.
• Checking for abnormalities by evaluating the quantity and quality of tears.

The type of blepharitis can be determined based on the appearance of the eyelid edges. If the symptoms frequently exhibited by the patients are mildly sticking eyelids, thickened lid margins, and missing/ misdirected eyelashes, then the type of blepharitis is diagnosed as Staphylococcal.

If the patients show mild redness of the eyelids or scales around the base of eyelashes, then it diagnosed as a Seborrheic blepharitis.
When the patient is found with blockage of the Meibomian Glands in the eyelids, poor quality of tears, and redness of the lining of the eyelids, Meibomian blepharitis is diagnosed.
If a hard, matted crust is formed on the eyelashes, and after its removal small sores appear on the skin, Ulcerative blepharitis is diagnosed.
In this case, patients may experience distortion of the front edges of the eyelids, loss of eyelashes, and chronic tearing. In severe conditions, keratitis is also present.
WHAT IS DEMODEX BREVIS?
Demodex brevis is a kind of mite found on the skin of humans.
Like its counterpart Demodex folliculorum, D. brevis is naturally occurring. D. brevis is so small that mitas can’t be seen macroscopically.
EXAM DESCRIPTION: MD LUCA VIGO SUGGESTIONS
Suggestions for diagnosis and treatment based on clinical procedure by Dr. Luca Vigo and studio carones (Milan, Italy).

A complete and dry eye-focused database allows to understand and properly diagnose the dry eye patient. With the useful data result tab, the ophthalmologist can check the complete tear film assessment, determining all deficiencies that cause the pathology and meantime understanding which treatment is needed to approach each case.

DIAGNOSIS SUGGESTION
Ocular surface data and pathology classification
Thanks to Studio Medico Carones with MD. Luca Vigo’s experience, TFA includes a suggestion algorithm able to share a possible treatment approach for each patient.
All suggestions can be useful for diagnosis and treatment.

TREATMENT MANAGING
Through TREATMENT MANAGING tab, the software allows the physician to fill in the database with all drugs, integrators and treatmenrs available in his practice.
Any treatments as vitamins, Omega-3, eye drops, hot packs and IPL/Radiofrequency, can be loaded on the software to prescribe the products of the brands that the doctor prefers.
The whole report with the diagnosis and treatment suggested by the ophthalmologist will be printed directly.

PROTOCOL
(MD L.VIGO Studio Carones Milano) is already provided and suggest treatment on our KOL experience.

All users can customize their own protocol adding treatment procedure to be chosen automatically right after performing the exams (this makes it possible as well to delegare the diagnosis to an assistant).
OTHER POSSIBLE EXAMINATIONS

AN ASSESSMENT OF GRADING SCALES FOR MEIBOGRAPHY IMAGES
The evaluation of the Meibomian Gland dysfunction appears to be of increasing interest in research and clinical practice. Consequently, the evaluation of MGs morphology using Meibography is of high interest for both researchers and clinicians.

WHITE TO WHITE MEASUREMENT
Evaluation of corneal diameter from limbus to limbus (white-to-white distance, WTW).
BULBAR REDNESS CLASSIFICATION
Acquiring an image of the conjunctiva, it will be possible to compare the patient’s condition with different international grading scales.


PUPILLOMETRY
The measurement of the pupil diameter has become increasingly important in the field of refractive surgery.
Larger scotopic pupil sizes may be partially responsible for the occurrence of postoperative symptoms such as halos, glare, and monocular diplopia.
Refractive surgeons also need an accurate scotopic pupil measurement to determine appropriate treatment zones for excimer laser, corneal, and intraocular surgery.

COMPARISON WITH THE MAIN INTERNATIONAL GRADING SCALES
EFRON - CCLRU - JENVIS - GLAUCOMA - FERNING TEST - MEIBOGRAPHY

DIFFERENT REPORTS AVAILABLE
The TFA software is a dedicated platform for dry eye and allows, in addition to helping in the diagnosis and classification of diseases, to print and save various medical reports, offering the most professional and clinical solutions to patients.
For customer satisfaction, it is often advisable to provide technical documentation relating to the exams taken.
Thanks to the various print reports of the Sapphire A+ device, you will have the possibility to visually explain and simply demonstrate the pathology situation. Furthermore, it’s possible to explain how the pathology has changed over time.
The TFA software is a dedicated platform for dry eye and allows, in addition to helping in the diagnosis and classification of diseases, to print and save various medical reports, offering the most professional and clinical solutions to patients.
For customer satisfaction, it is often advisable to provide technical documentation relating to the exams taken.
Thanks to the various print reports of the Sapphire A+ device, you will have the possibility to visually explain and simply demonstrate the pathology situation. Furthermore, it’s possible to explain how the pathology has changed over time.

COMPLETE REPORT
Complete report with all results and pictures used to explain to the patient any dry eye category.

TREATMENT REPORT
Patient oriented report explaining causes of pathology and recommended treatments.

FOLLOW UP REPORT
For each value it is possible to show the trend line before/during/after treatment.

DAILY REPORT
Brief single page report to show at a glance all exams results.

MONOCULAR REPORT
To save and prind one only interesting examination.

BINOCULAR REPORT
To save in a single pdf the same eamination of both eyes.
Reports
The Sapphire A+ device provides 3D imaging, to help you explain the cause of dry eye and assist your recommendations for treatment. It gives you the ideal tool to easily explain what the cause of the patients’ eye discomfort is, while helping each patient to understand where your recommendation is coming from.
The Sapphire A+ device means you can offer peace of mind to your patients, with the knowledge that you are using the latest technology for correct diagnosis and treatment.
Video Sapphire A+
Sapphire - Dry Eye Disease
| Image Resolution | 5 MP |
| Acquisition Mode | Multi shot, video |
| Focus | Autofocus, manual focus |
| ISO Management | Variable |
| Cones | Main cone and Placid cone |
| Camera |
Colored, sensitive to infrared
(NIR), yellow-filtered |
| Light Source | Infrared LED – Blue, red and white LED |
| Image Resolution | 5 MP |
| Acquisition Mode | Multi shot, video |
| Focus | Autofocus, manual focus |
| ISO Management | Variable |
| Cones | Main cone and Placid cone |
| Camera |
Colored, sensitive to infrared
(NIR), yellow-filtered |
| Light Source | Infrared LED – Blue, red and white LED |
Sapphire Catalog 2022
Dry Eye Disease - Essential Information
Dry Eye - The impact of Dry-Eye on cataract and refraction surgery
Sapphire - Fully Automatic Dry Eye Diagnostic Platform
Sapphire - Patient Information
Sapphire - Reports
Article 1 - A review of meibography for a refractive surgeon
Article 2 - Ocular Surface Workup With Automated Noninvasive Measurements for the Diagnosis of Meibomian Gland Dysfunction
Article 3 - Noninvasive ocular surface analyzer as an adjunct in diagnosis and estimating prevalence of meibomian gland dysfunction: Hospital‑based comparative study
Article 4 - Algorithmic approach to diagnosis and management of post-refractive surgery dry eye disease
Article 5 - Real-World Diagnostic Performance of a Novel Noninvasive Work-up in the Setting of Dry Eye Disease Journal
Article 6 - Qualitative assessment of the tear film in young adults
Article 7 - Analysis of two latest generation in-office therapies for the treatment of dry eye
Dr. Sergio M. Solarino

Dr. Francesco Carones

Dr. Massimo Gualdi

Dr. Luca Gualdi

Dr. Eros Radrizzani

Dry Eye Disease - Sapphire
Establishing a Treatment Protocol - Sapphire
Patient Smartphone Application - Sapphire
Overview of Examination - Sapphire
Understanding NIBUT - Sapphire
Blink Quality - Sapphire