PERIMETRY PRINCIPALS
Perimetry principals focuses on all essential functions and provides meaningful clinical guidance to assist Ophthalmologists and Optometrists to achieve fast and clinically relevant eye examinations and optimal clinical outcomes for patients.
PERIMETRY
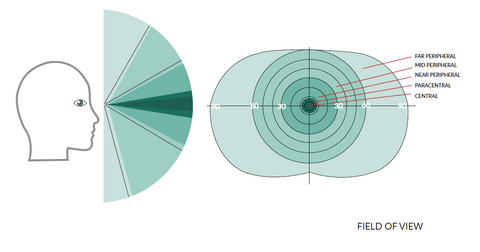
Perimetry is one of the most common eye examinations performed by eye health care professionals. The aim of perimetry is to examine the field of view (area that is seen by the eye) and evaluate eye health and assist in the early detection of emerging eye disease or manage existing disease progression such as glaucoma and neurological disorders. Perimetric tests are fast and painless, and are a vital diagnostic tool used worldwide.
MAIN PURPOSE
The evolution of perimetry technology makes it possible to perform the examination more precisely and faster than even before. Technological improvements in the detection of visual loss allows eye health care professionals to identify disease earlier and monitor losses over time.
COMMON PERIMETRY DIAGNOSTICS INCLUDE
Glaucoma can be detected in early stages using Static perimetry, the gold standard for detecting disease progression of Glaucoma.
Neurological changes exhibit characteristic results like local defects, islands in the field of view, especially optic nerve diseases.
Retinal disfunction including local detached retinas, delamination and age-related macular degeneration.
Perimetry is commonly performed when the patient presents with symptoms on unknown etiology:
- Low visual acuity,
- Hypertension,
- Headache of unknown origin.
PERIMETRY EXAMINATION ENABLES
- Binocular examination to determine visual field health or emerging defects, a common requirement for professional drivers.
- Certain industries that require individuals to undertake special tasks often require regular eye heath examination, as part of broader Industrial Medicine strategy, necessary for work place employment.
TYPES OF PERIMETRY
STATIC
Most commonly used and by eye health professionals called the modern gold standard. Test points (stimulii) are displayed in certain positions for a pre-programmed time. Patient simply reacts by pressing a response button when he/she can see the LED stimulus.
KINETIC
This capability exclusively designed for manual perimeters. Stimulus is displayed peripherally in the bowl and moves with a constant speed into the bowl centre. Patient clicks the response button when he/she can see the stimulus.
Kinetic perimetry provides preliminary approximation of a field of view, rather outer field borders, where static perimetry provides a more detailed analysis of fieldof view.
Considered useful for testing elderly or handicapped patients.
FIELD OF VISION
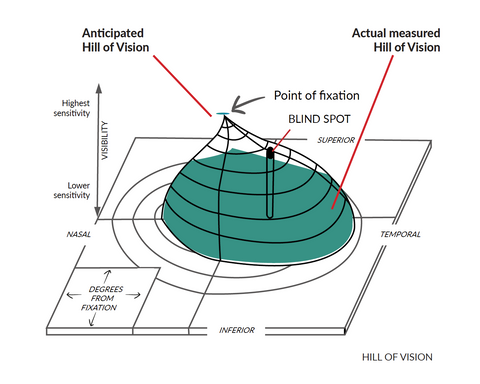
Normal field of vision has a shape commonly known as Hill of Vision.
Retina sensitivity is highest across central field of view and decreases peripherally. If the patient’s retina does not react as clinically anticipated, the Hill of Vision is decreased in certain area or multiple areas. In the example below, central field of vision is lowered.
MEASUREMENT BASICS
ILLUMINATION
Perimeter bowl projects continuous LED illumination and automatically changes intensity if ambient light conditions affect the illumination levels required to complete an examination. Stimulus is displayed as a light spot with a constant colour and size, but with different intensity. Stimulus intensity is expressed in decibels. 0dB (zero) = the highest possible intensity, where 36dB = very low intensity.
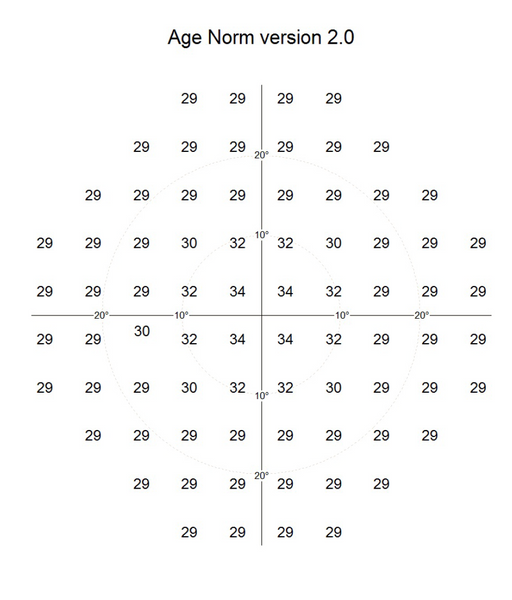
AGE NORMAL FIELD OF VIEW
Retina sensitivity is higher in the centre, lower in the periphery. Retinal sensitivity decreases with age.
These long understood clinical assumptions allow eye health professionals to measure Age Normal field of view.
- Age Normal are statistical measured values defining the lowest stimulus intensity which should be seen by person belonging to a particular age group.
- Age Normal values are statistical references if patient test result is correct or incorrect.
- Age Normal values are used as initial test values for certain strategies (Screening, Fast Threshold, Threshold).
There are different clinical methods for examinations known as Strategies. There are also different test field shapes. Test field can cover whole field of view or only the part of it. In addition, different stimulus sizes and colours can be used. Combinations of these reference to the appropriate Age Normal fields of view.
EXAMPLE
Age Normal values for AP-300 in decibels: higher values are in the centre, sensitivity decreases in the periphery.
30-2 test field
THE EXAMINATION
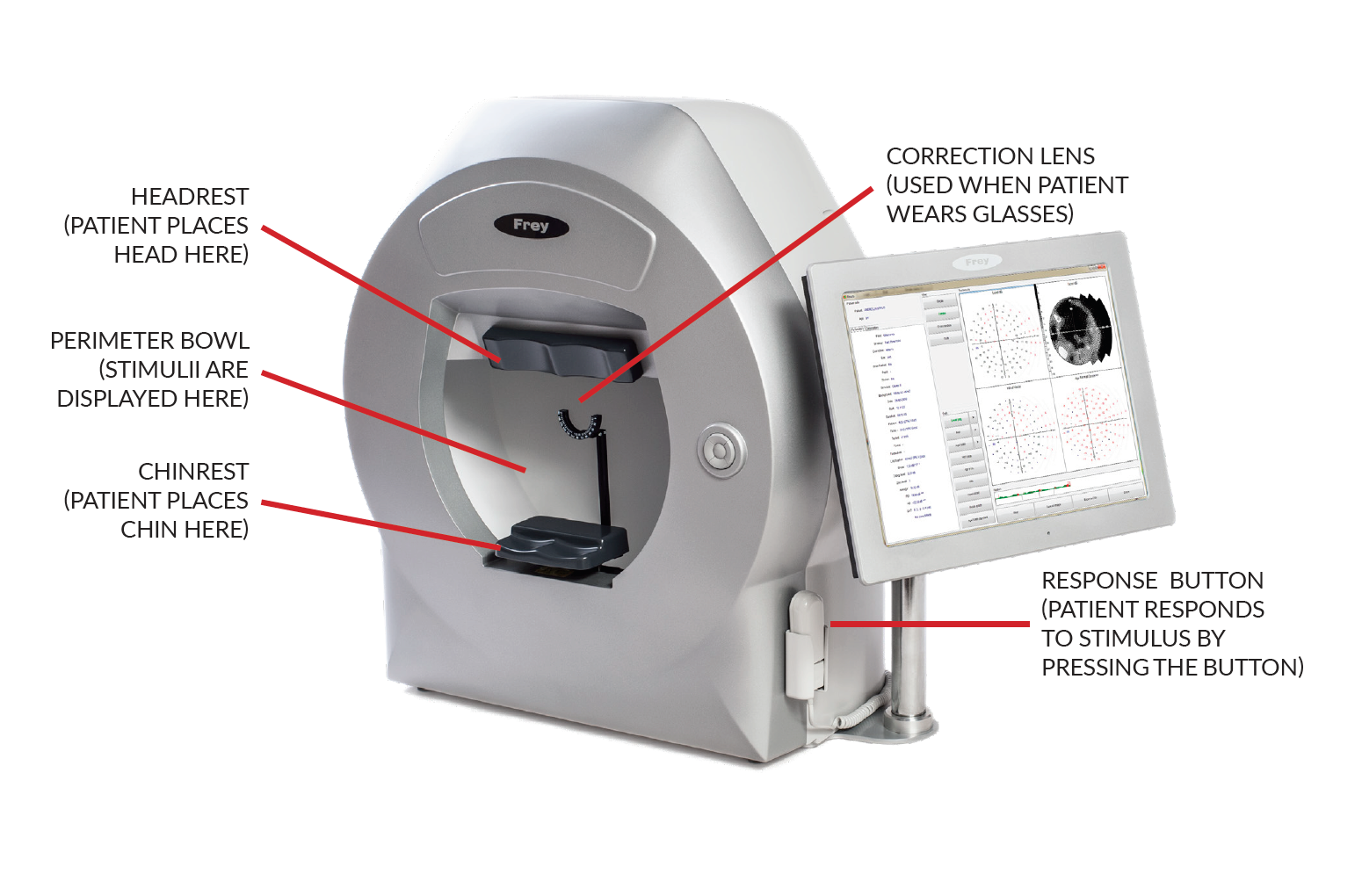
HOW PERIMETRY TEST IS CONDUCTED?
Humans are subjectively convinced that they have good eyesight and they can see everything. Therefore, it is commonly difficult for humans to be objective, espe-cially with changes in our field of view. Only when a significant change or defect in filed of view occurs appears, humans develop a sense of narrowed or tunnel vision.
BEFORE THE EXAMINATION
PATIENT DEMO – undertake a demonstration examination prior to clinical examination to familiarize the patient with the device, respond to questions and allay patient anxiety. Following this simple introduction will increase patient comfort and cooperation and improved clinical examination outcome. Prior to clinical examination instruct the patient how to sit in front of the device, upright posture and relax during the examination. Remind the patient to visually focus on LED fixation point (without moving the eyeball from side to side). It is OK to blink as required.
GLASSES and CONTACT LENSES – if the patient uses glasses every day, the examination should be undertaken with spectacle correction with which the patient can see sharply from a distance of 30 cm.
IMPORTANT NOTE
- It is very important that during the entire examination the patient looks at the fixation point located in the central part of the perimeter’s bowl.
- Examination room must be darkened.
- Avoid filtered light and unnecessary distractions during the examination for optimal clinical outcomes.
DURING THE EXAMINATION
- Left and right eyes are tested separately as two independent examinations.
- Each eye examination will last several minutes depending on the strategy chosen.
- Patient positioning is correct with comfortable chin and head rest and views into the perimeter bowl while observing one (1) particular point known as fixa-tion point.
- Multiple stimuli (LED lighting) are displayed diffusely across the perimeter bowl’s surface with differing light intensities.
- Patient activates the response button when the patient visualizes the LED stimulus on the surface of the perimeter’s bowl.
VISUAL FIELD STRATEGIES
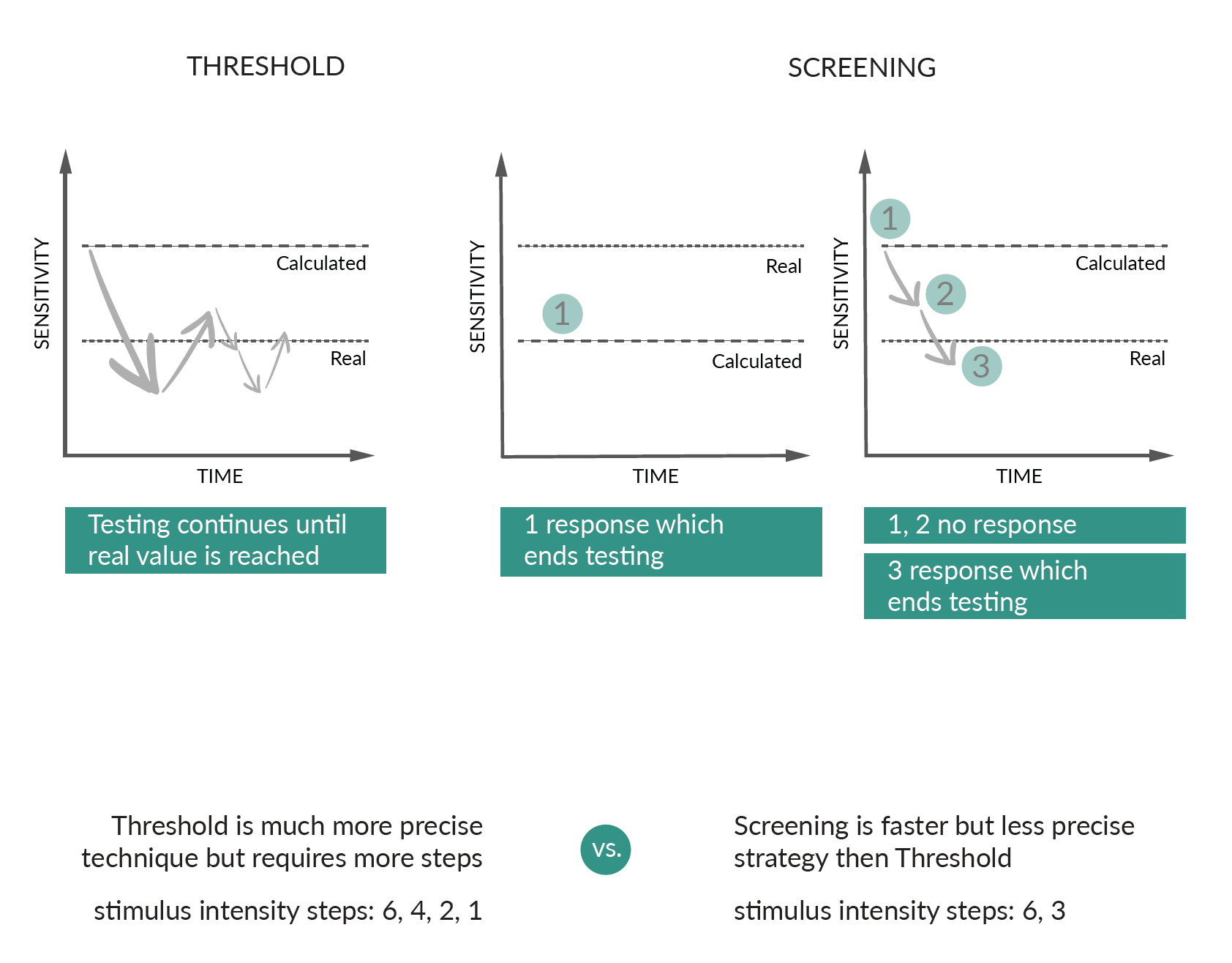
Method of conducting examination, how points are displayed, is known as ‘strategy’. There are three (3) groups of strategies:
- Threshold strategies,
- Screening strategies (Suprathreshold),
- Special strategies (derivatives of screening strategies).
Screening strategies are used for fast and superficial checking if a patient’s vision is not affected in comparison with appropriate age norm.
Perimeter LED displays dB brighter than Age Norm value for this point.
- If patient can see this point, examination is completed. Actual sensitivity is not reached at this point, the information that patient is above Age Norm value is clinically satisfactory.
- If patient cannot see this point, perimeter decreases the stimulus intensity by 3dB until patient reaches intensity level when point is seen.
Threshold strategies are used for detailed examination of a patient’s vision in order to diagnose possible defects, for example glaucoma disease and retina health.
Perimeter LED displays dB darker than Age Norm value for point #1.
- If patient cannot see this point, perimeter increase the stimulus intensity by -4dB #2.
- If patient cannot see point #2 perimeter again increases stimulus intensity by -4dB #3.
- If patient can see point #3 perimeter decreases the stimulus intensity by 2dB #4.
- If patient can see point #4 perimeter decreases the stimulus intensity by 1dB #5.
This method is called ‘threshold bracketing’ and provides 1dB accuracy, demonstrating actual real sensitivity patient vision.
Strategy defines how quickly and precisely retina sensitivity will be measured.
TEST RESULTS
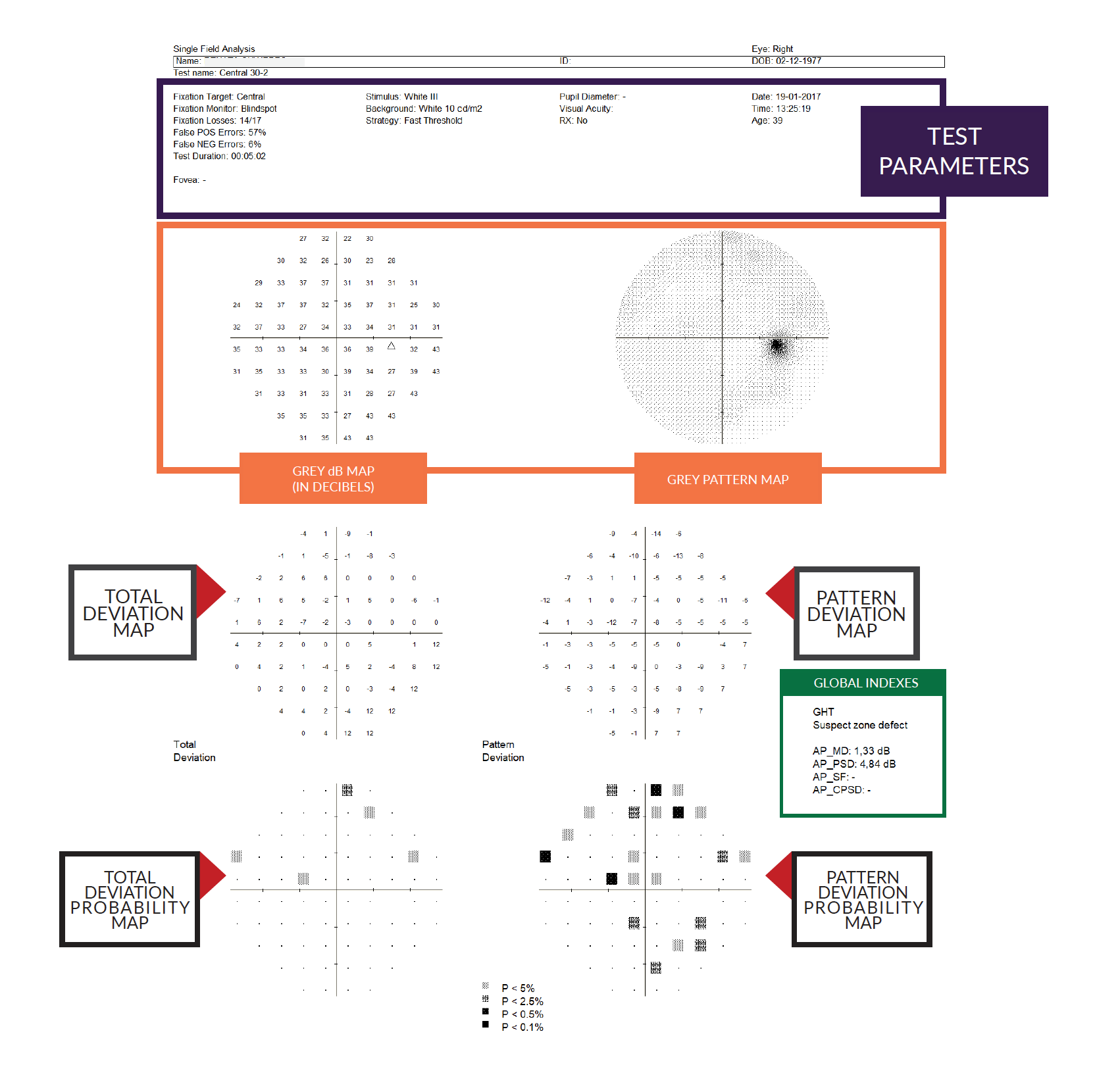
INFORMATION ABOUT PRINTOUTS
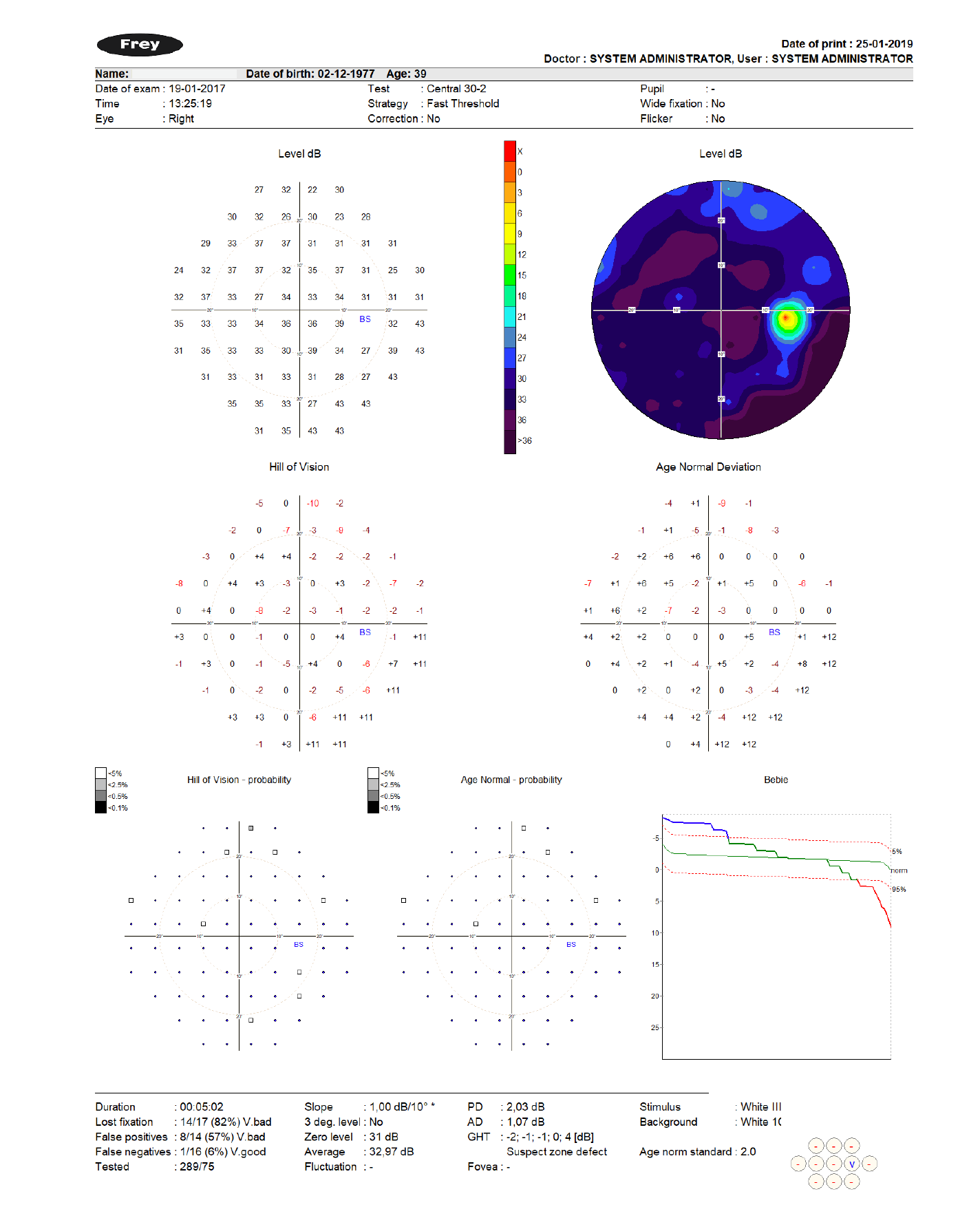
The most used printout format is called ’Standard HFA’ and is compatible with standard introduce by Zeiss Humphrey in their HFA perimeters line.