Glaucoma is the leading cause of blindness in people over the age of 60. Blindness due to glaucoma can often be prevented if treated early.
What is the main cause of glaucoma?
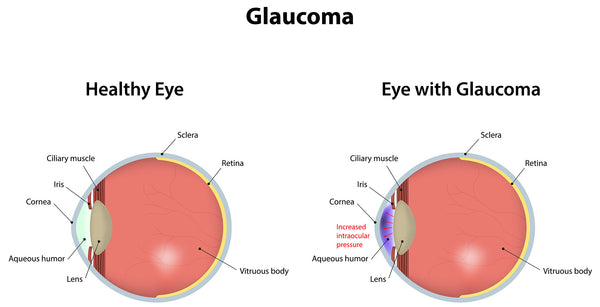
The eyes constantly produce aqueous humor. When new aqueous fluid enters the eye, the same amount must be expelled. The fluid drains through an area known as the drainage angle. This process keeps the pressure in the eye (called intraocular pressure or IOP) stable. However, if the drainage angle is not correct, the fluid can accumulate, resulting in increased pressure inside the eye, which can damage the optic nerve. Improper drainage angle is a risk factor for glaucoma in otherwise healthy eyes.
In a healthy eye, fluid flowing out through the drainage angle maintains a stable pressure.
The optic nerve is composed of over one million tiny nerve fibers, resembling an electrical cable with numerous small wires. When these nerve fibers die, blind spots develop in your vision. Often, these blind spots go unnoticed until a significant number of optic nerve fibers have died. Complete loss of all fibers results in blindness.
How does glaucoma develop?
There are two main types of glaucoma.
- Chronic open-angle glaucoma: This is the most common type, developing gradually when the eye's drainage of fluid becomes inadequate, similar to a clogged drain. Consequently, eye pressure increases and begins to damage the optic nerve. Initially, this type of glaucoma is painless and doesn't cause changes in vision.
In some individuals, the optic nerve may be more sensitive to normal eye pressure, putting them at higher risk for glaucoma. Frequent eye examinations are essential to detect early signs of optic nerve damage.
- Angle-closure glaucoma (also known as "narrow-angle glaucoma"): This type occurs when a person's iris is positioned very close to the drainage angle in the eye, potentially obstructing it. It is akin to a piece of paper blocking a sink's drain. When the drainage angle is completely blocked, eye pressure rapidly increases, resulting in an acute attack. This constitutes a true eye emergency, requiring immediate consultation with an ophthalmologist, as it can lead to blindness.
The following are signs of an acute attack of angle-closure glaucoma:
- Sudden blurry vision
- Severe eye pain
- Headache
- Stomach pain (nausea)
- Vomiting
- Seeing rings or rainbow haloes of color around lights
Many individuals with angle-closure glaucoma develop it gradually, referred to as chronic angle-closure glaucoma. In the beginning, there may be no symptoms, causing individuals to be unaware of their condition until the damage becomes severe or an acute attack occurs.
Angle-closure glaucoma can cause blindness if not promptly treated.
Symptoms of glaucoma
Open-angle glaucoma: During the early stages of open-angle glaucoma, there are usually no obvious symptoms or warning signs. As the disease progresses, blind spots develop in the peripheral (side) vision.
Most individuals with open-angle glaucoma do not notice any changes in their vision until the damage is severe. This is why glaucoma is often referred to as the "silent thief of vision." Regular vision screenings can help your ophthalmologist detect the disease before vision loss occurs. Your eye doctor can provide guidance on the recommended frequency of examinations.
Angle-closure glaucoma: People at risk of developing angle-closure glaucoma typically do not exhibit symptoms before an attack. Some initial symptoms of an attack may include blurred vision, halos of light, mild headaches, or eye pain. Individuals experiencing these symptoms should seek immediate examination by an ophthalmologist. An attack of angle-closure glaucoma is characterized by the following symptoms:
- Severe pain in the eye or forehead
- Redness of the eye
- Decreased or blurred vision
- Seeing rainbow-like halos of light
- Headache
- Nausea
- Vomiting
Normal-tension glaucoma: Individuals with normal-tension glaucoma have eye pressure within the normal range, but show signs of glaucoma such as blind spots in their field of vision and optic nerve damage.
Do glaucoma suspects have symptoms? Some individuals show no signs of damage but have higher than normal eye pressure, a condition known as ocular hypertension. These patients are considered "glaucoma suspects" and have an increased risk of developing glaucoma. Others may be considered glaucoma suspects even with normal eye pressure, if their ophthalmologist observes something different about their optic nerve. Individuals suspected of having glaucoma should undergo careful evaluation by their ophthalmologist to monitor any changes over time and initiate treatment if necessary.
Symptoms of pigmentary dispersion syndrome and pigmentary glaucoma: Pigmentary dispersion syndrome (PDS) occurs when pigment from the back of the iris rubs off and can elevate eye pressure, potentially leading to pigmentary glaucoma. Some individuals with PDS or pigmentary glaucoma may experience halos or blurred vision after certain activities like jogging or playing basketball.
If you experience any of these symptoms or other concerning changes in your vision, it is important to consult with your ophthalmologist for proper evaluation and guidance.
Who is at risk for glaucoma?
Some individuals are at a higher than normal risk for glaucoma. This includes people who:
- are older than 40
- have relatives with glaucoma
- are of African, Hispanic, or Asian descent
- have high eye pressure
- are farsighted or nearsighted
- have suffered an eye injury
- have a history of long-term steroid use
- have thin corneas
- have narrowing of the optic nerve
- have diabetes, high blood pressure, migraines, poor blood circulation, or other systemic health problems that can affect the entire body.
Talk to your ophthalmologist about your risk for glaucoma. People who have more than one of these characteristics are at an even greater risk for glaucoma.
How is glaucoma diagnosed?
The only definitive way to diagnose glaucoma is through a comprehensive eye exam. Relying solely on a glaucoma test that checks eye pressure is not sufficient for diagnosing glaucoma.
During a glaucoma exam, your ophthalmologist will:
- measure your eye pressure
- evaluate the drainage angle of your eye
- examine the optic nerve for any signs of damage
- test your peripheral (side) vision
- take images or measurements of the optic nerve
- measure the thickness of the cornea
Glaucoma is often referred to as the "silent thief of sight" because it typically has no symptoms in the early stages. In fact, around half of people with glaucoma are unaware that they have the condition. Regular eye exams play a crucial role in detecting the disease before it progresses to blindness. Your eye doctor can advise you on the recommended frequency of testing.
Can glaucoma be stopped?
Glaucoma damage is permanent and cannot be reversed. However, it can be halted or slowed down through medication and surgery. Your ophthalmologist may employ one or more of the following treatments to manage glaucoma:
Glaucoma medications: Eye drops are commonly used to control glaucoma. These drops, which are applied daily, help reduce the pressure inside the eye. Some medications achieve this by decreasing the production of aqueous fluid, while others improve its drainage through the angle.
It's important to note that glaucoma medications may have side effects, such as itching or stinging sensations, redness of the eyes or surrounding skin, changes in pulse and heart rate, changes in energy level, changes in breathing (especially for individuals with asthma), dry mouth, blurred vision, eyelash growth, and changes in the color or appearance of the eyes or eyelids.
All medications carry potential side effects, and some may interact with other medications. Make sure to inform your doctor about all the medications you are taking. If you experience any side effects from your glaucoma medication, contact your eye doctor, but never stop or alter the medication without consulting your ophthalmologist. If your prescription is running low, consult with your ophthalmologist regarding refills.
Laser surgery: There are two primary types of laser surgery used to treat glaucoma. These procedures aid in improving the drainage of aqueous humor from the eye and are typically performed in the ophthalmologist's office or outpatient surgery centers.
Trabeculoplasty: This surgery is intended for individuals with open-angle glaucoma and may be performed as an alternative or addition to medication. The surgeon utilizes a laser beam to enhance the functionality of the drainage angle, allowing the aqueous humor to flow properly and reducing the intraocular pressure.
Iridotomy: This procedure is performed on individuals with angle-closure glaucoma. The ophthalmologist uses a laser beam to create a small hole in the iris, facilitating the flow of aqueous humor into the drainage hole.
Surgery in an operating room
Certain glaucoma surgeries are conducted in an operating room. These procedures involve creating a new drainage pathway for the aqueous humor to exit the eye.

Trabeculectomy: In this procedure, the eye surgeon creates a small flap in the sclera (the white part of the eye) and forms a concealed pocket called a bleb within the conjunctiva (the thin membrane covering the inside of the eyelids and the whites of the eyes). The aqueous humor can drain out of the eye through the flap and into the bleb, where it is absorbed by the surrounding tissue, effectively reducing the intraocular pressure.
Glaucoma drainage devices: In some cases, your ophthalmologist may implant a small drainage tube in your eye to redirect the fluid to a reservoir. The surgeon creates this reservoir beneath the conjunctiva, and the fluid is subsequently absorbed into the nearby blood vessels.
Cataract surgery: For individuals with narrow angles, removing the eye's natural lens through cataract surgery can help lower the intraocular pressure. Narrow angles occur when the iris and cornea are in close proximity, obstructing the drainage channel of the eye. Removing the lens creates more space for the fluid to drain.
Your role in glaucoma treatment
Successful glaucoma treatment requires collaboration between you and your doctor. Your ophthalmologist will prescribe the appropriate glaucoma treatment, typically in the form of eye drops. It's essential to use the drops as directed.
Upon initiating glaucoma medication, your eye doctor will likely schedule more frequent follow-up appointments, typically every 3 to 6 months, although the frequency may vary based on your specific treatment needs.
If you have any questions about your eyes or treatment, don't hesitate to discuss them with your ophthalmologist.





